An Atypical mole, also called a dysplastic nevus, is a benign growth that may share some of the clinical or microscopic features of melanoma, but is NOT a melanoma or any other form of cancer. However, the presence of atypical moles may increase the risk of developing a melanoma and is used as a marker for someone who is at risk of developing melanoma. This increased risk varies from very small for those with a single atypical nevus to higher for those with many.
Dysplastic nevi have some of the ABCD characteristics and can look like a melanoma. These features are:
- Asymmetry – One half of the mole doesn’t match the other half.
- Border irregularity – The edges are ragged, notched or blurred.
- Color – The color is not uniform, shades of tan, brown, and black are present (rarely red, white & blue)
- Diameter – The width is greater than six millimeters (size of a pencil eraser) or growing rapidly.
When dysplastic nevi are biopsied and looked at under a microscope, they have a certain pattern that allows the pathologist to make the diagnosis and exclude melanoma. Dysplastic nevi may occur anywhere on the body (even non-sun-exposed places), but are more prevalent on sun exposed areas of the body, back and legs.
What does it mean if I have a single atypical nevus?
The lifetime risk of a person in the U.S. developing melanoma is 1 in 70. A patient with one to four atypical nevi without a personal or family history of melanoma is at a slightly higher risk than the general population. Atypical nevi should be observed for changes, biopsied or conservatively excised.
What does it mean if I have many moles and atypical nevi?
The risk of developing melanoma is higher if a patient with many atypical nevi has a personal or family history of melanoma. If so, their family may have Familial Atypical Mole Syndrome. A person who fits this criteria has:
- A relative (e.g., parent, sibling, child, grandparent, aunt, or uncle) with melanoma.
- A large number of moles, more than 50, some of which are atypical.
- Nevi that demonstrate certain microscopic features found during a biopsy.
Patients who fit this criteria have a higher risk for melanoma and need to do self skin exams (see below) every two to three months. They should have a complete skin exam by their dermatologist every 3 to 12 months. The goal is to permit early detection of melanoma, should it occur. The most important step you can take is to check your skin. If the appearance of a mole worries you or it changes suddenly, you should consult a dermatologist.
What can I do to prevent the development of melanoma?
Overexposure to sunlight is the main cause of melanoma. Although any race can get melanoma, fair skinned people living in sunny climates have a much higher risk (Arizona has the 2nd highest incidence of skin cancer in the world). Following these steps can help reduce your risk of developing melanoma.
- Seek shade or stay indoors between 10am – 4pm
- Wear light colored, tightly woven protective clothing and wide brim hats (3 inches)
- Apply sunscreen with SPF of at least 15 – 30 to exposed areas. Reapply every hour. (Note: Sunscreens are not perfect and cannot block all the sunrays, so do not use them as an excuse to spend more time in the sun)
- Perform self-skin exams every 2-3 months (see below)
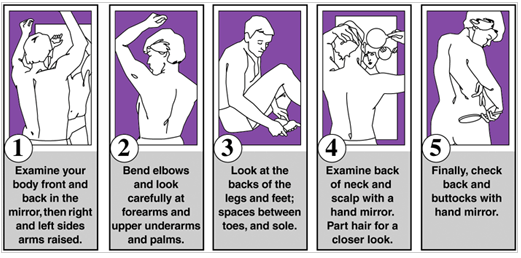
Periodic Self-Examination – Prevention of melanoma/skin cancer is the best weapon against these diseases. But if a melanoma should develop, it is almost always curable if caught in the early stages. Practice periodic self-examination to aid in early recognition of any new or developing lesion. The following is one way of self-examination that will ensure that no area of the body is neglected. To perform your self-examination you will need a full length mirror, a hand mirror and a brightly-lit room.